Medical Billing Services
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for medical services rendered. This process can be complex and time-consuming, requiring a thorough understanding of medical codes, insurance policies, and billing regulations.
The first step in medical billing is to gather all relevant patient information, such as demographics, insurance details, and medical history. This information is used to create a patient file and ensure that all billing is accurate and complete.
Once the patient information is gathered, the healthcare provider will provide a bill for services rendered. This bill will typically include a breakdown of all services provided, along with the corresponding medical codes used to identify each service. These codes are standardized and are used by insurance companies to determine coverage and payment amounts.
After the bill is submitted, the insurance company will review the claim to determine if it meets the policy requirements for coverage. If the claim is approved, the insurance company will issue payment to the healthcare provider. However, if the claim is denied, the healthcare provider will need to follow up with the insurance company to determine the reason for the denial and take appropriate action to correct the issue.
Medical billing can be a complicated and time-consuming process, and many healthcare providers choose to outsource this function to specialized billing companies. Telaka Health has the expertise and resources needed to handle all aspects of medical billing, from initial claim submission to follow-up on denied claims.
Overall, medical billing is a critical function for healthcare providers and requires specialized knowledge and expertise to ensure accurate and timely payment for services rendered. Our company has the the solid understanding of medical codes, insurance policies, and billing regulations to ensure a smooth and efficient billing process.
What Is Revenue Cycle Management?
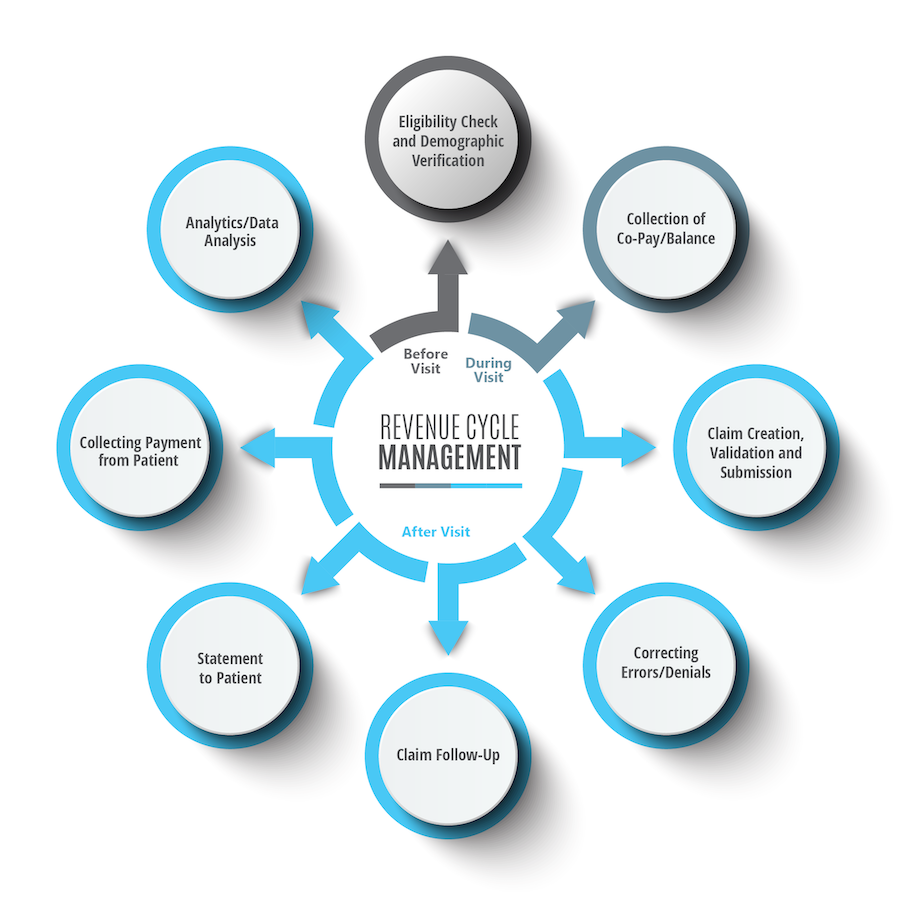
Revenue Cycle Management (RCM) is an important, financially-driven process in healthcare that allows providers to receive reimbursement for care delivery in a timely and efficient manner.
An effective RCM process ensures that the full interaction with a patient from initial inquiry through final payment is effectively managed. This means that appropriate information is collected and documented, patients are only billed for services provided, third-party payers are contacted in a timely manner and payments are collected.
How we can help.
Telaka Health excels in the realm of medical billing, offering a diverse array of services tailored to meet the specific needs of healthcare providers and streamline their billing processes. Our comprehensive suite of services includes
- Claims submission: A medical billing company can handle all aspects of claims submission, including data entry, medical coding, and submission to insurance companies.
- Claims follow-up: If a claim is denied or rejected, a medical billing company can follow up with the insurance company to determine the reason for the denial and take appropriate action to correct the issue.
- Insurance verification: A medical billing company can verify patient insurance coverage and eligibility before submitting claims, reducing the risk of claim denials and delays.
- Revenue cycle management: A medical billing company can manage the entire revenue cycle process, from initial patient registration to final payment collection.
- Reporting and analytics: A medical billing company can provide detailed reports and analytics on the healthcare provider’s billing performance, including claims submission rates, denial rates, and revenue trends.
- Compliance support: A medical billing company can provide guidance and support to ensure that healthcare providers are compliant with all billing regulations and requirements.
Telaka Health offers tailored solutions to streamline billing processes, alleviate administrative burdens, and bolster revenue collection for healthcare providers. By entrusting their billing needs to our dedicated specialists, providers can redirect their focus towards delivering exceptional patient care, knowing that the intricacies of billing management are in capable hands.
Address
Telaka Health
1222 Professional Blvd Suite B
Evansville, Indiana
Connect
E: info@telakahealth.com
© 2024 Telaka Health