Medical Credentialing Services
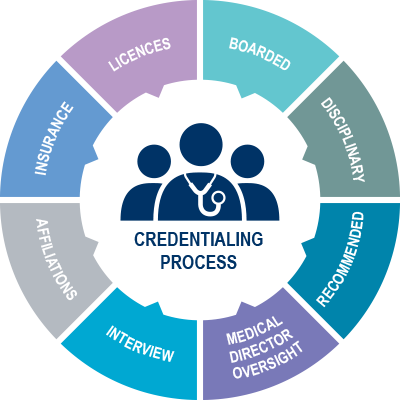
Credentialing serves as the cornerstone in the healthcare industry, acting as a meticulous process through which healthcare facilities rigorously assess and confirm the qualifications of prospective medical practitioners before welcoming them into their teams. This multifaceted system is designed to provide a comprehensive verification of a healthcare provider’s credentials, encompassing not only licenses and certifications but also a thorough evaluation of their training, expertise, and professional background.
By meticulously verifying the qualifications and credentials of medical professionals, credentialing ensures that healthcare organizations maintain the highest standards of care delivery and patient safety. It acts as a safeguard, assuring both the healthcare institution and the patients that the practitioners possess the requisite skills and knowledge to offer optimal medical services.
Furthermore, credentialing offers a sense of assurance and confidence to patients, affirming that they are entrusting their well-being to certified and competent healthcare professionals. It serves as a tangible manifestation of a practitioner’s commitment to ongoing learning and adherence to industry best practices, thereby fostering trust and transparency in the patient-provider relationship.
In essence, credentialing not only validates the expertise and qualifications of healthcare practitioners but also plays a pivotal role in upholding the integrity and quality of healthcare delivery, ultimately contributing to improved patient outcomes and satisfaction.
The Importance of Credentialing.
Delays or lapses in the credentialing process not only disrupt the operational flow of healthcare facilities but can also create significant financial strains. When reimbursements are delayed or denied due to incomplete or inefficient credentialing, it directly impacts the revenue stream of healthcare providers. Such interruptions can impede the ability to cover operational costs, invest in essential resources, and even jeopardize the quality of patient care.
Provider credentialing is undeniably pivotal, yet navigating its complexities requires a seasoned professional well-versed in its intricacies. Without the expertise to maneuver through the intricate web of licensure requirements, certifications, and compliance standards, healthcare organizations may find themselves caught in a bureaucratic quagmire, leading to prolonged delays and missed opportunities for reimbursement.
Attempting to tackle credentialing internally can quickly become a burdensome ordeal for healthcare staff. The process demands meticulous attention to detail, consumes valuable time, and diverts focus away from core patient care responsibilities. Staff members, already stretched thin by their existing duties, may find themselves overwhelmed by the sheer volume of paperwork, verifications, and follow-ups required to ensure credentialing compliance.
At Telaka Health, we recognize the challenges posed by the credentialing process and offer a comprehensive solution to alleviate the burden on healthcare providers. With our experienced team handling every aspect of credentialing, from initial applications to ongoing maintenance, we ensure a seamless and efficient process that prioritizes accuracy and timeliness. By entrusting Telaka Health with your credentialing needs, healthcare facilities can redirect their focus back to what matters most – delivering exceptional care to their patients.
Address
Telaka Health
1222 Professional Blvd Suite B
Evansville, Indiana
Connect
E: info@telakahealth.com
© 2023 Telaka Health